Ventilation and air conditioning for medical institutions: rules and features of the arrangement of ventilation
Medical facilities are organizations in which special demands are made on air quality. Agree, it is impossible to imagine a clinic where ventilation does not function properly. Such a room is clearly a particular danger, since the air is literally saturated with various kinds of infections, bacteria, that is, you can’t enter such a hospital.
In addition, a number of drugs have a very strong smell, so you need to work with them exclusively with the hood turned on. In order for the medical institution to really be able to help patients, rather than provoke the development of new diseases, special requirements are provided.
The guidelines and recommendations that ventilation and air conditioning for medical facilities must comply with are discussed below. Also considered are the rules for arranging a ventilation system for individual rooms in a hospital, for example, an operating room or a doctor’s office.
The content of the article:
The need for ventilation in a hospital
Despite the fact that any clinic is a public place, it is medical institutions that have special air exchange requirements.

There are two types of ventilation - natural and artificial. The first is the one that occurs due to the difference in temperature in the room and outside the window. Also, natural ventilation can be carried out due to strong flows of air (wind).
The advantage of this type of air exchange is its availability and low cost. So, natural ventilation can be carried out by aeration, that is, ventilation. To do this, wide open windows, vents or doors, forming a draft.
An obvious minus of this method is the need for its prolonged use to completely update the composition of the air in the room. In addition, during aeration, a strong jet of cold air enters the room, which is simply unacceptable for some patients.
Therefore, ventilation and air conditioning for medical facilities are often based on artificial air exchange.
However, aeration is also used to this day, but in a strictly dosed amount. So, it is recommended to arrange the ventilation of all rooms in a medical facility at least 4 times every day. The duration of each aeration should not be less than 15 minutes.
An exception to this rule is all rooms with class “A” cleanliness:
- resuscitation;
- burn compartment;
- postpartum room;
- manipulative for newborns.
In such chambers, complete sterility is required, therefore ventilation in them is prohibited, and air exchange is based solely on artificial ventilation.
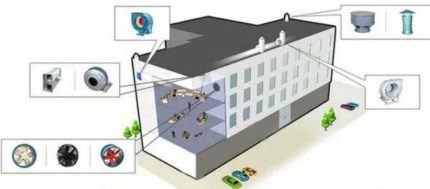
Principles of arranging artificial ventilation
This type of ventilation is based on the mechanical movement of air flows, due to the installation of special devices.
Depending on the purpose of ventilation, its types are distinguished:
- Supply - provides clean air to the room;
- exhaust - removes polluted air;
- mixed - provides air circulation.
For medical institutions, the installation of supply and exhaust ventilation is typical, but the air exchange in the rooms depends on the type of chambers.
So, for wards in which non-infectious patients are located or patients are only being treated, an equal inflow and exhaust are characteristic. Similarly, ventilation is also equipped in doctors' offices, where air exchange must be carried out constantly, due to the large number of patients.

Such ventilation is also established in the wards, where infected patients are treated and in purulent surgery.
Supply air prevails in rooms where increased sterility is needed. That is, where you need a constant supply of clean air. Such wards include resuscitation, a birth room, rooms where newborns are kept.
Another type of ventilation is called laminar air flow. This type of air exchange is used where you need a constant flow of clean air, which previously passes through an enhanced filtration system.

It is worth paying attention that aeration is prohibited in such chambers, and air flows, before being fed into the room, pass through the additional cleaning system.
There is ventilation, in which there is no influx of fresh air.
it is mounted in such rooms:
- restroom;
- shower room;
- a room for storing dirty linen (bedding, patients ’clothing, doctors’ smocks);
- in cabinets that are used to store reagents and disinfectants.
In all medical institutions, both air supply and removal are from the upper part of the room.
Air exchange in operating rooms
Organization of air exchange in the operating room is one of the important stages in the planning of this chamber.The fact is that one of the factors that makes surgical intervention successful is the increased sterility of all surfaces and air. Therefore, for ventilation design in operating rooms, the following standards and requirements should be observed.
In the area of the doors, a gateway with air pressure must be installed. This is done in order to exclude the ingress of untreated air flow from the corridor, elevator, etc.
In the operating room itself, ventilation should provide such a volume of fresh air inflow that its amount is at least 15% greater than those air masses that the hood removes. Due to such a system creates air backwater.
Therefore, the purified air circulates not only in the operating room, but also extends to the preoperative and postoperative.
In separate operating rooms in which such surgical interventions are performed that require increased sterility (heart or brain surgery), a laminar air flow is provided. Due to this, such an exchange of air is achieved, which is 500-600 times higher than that which is possible with the arrangement of conventional ventilation.
When designing ventilation in the operating room, it is necessary to provide for its operation in emergency mode. That is, if the main part is disconnected due to power outages or fails, it should be automatically replaced by a spare one.
The value of microclimate for medical institutions
Given the fact that hospitals receive those who need medical care, and those in the wards who receive it, it is worthwhile to carefully monitor the observance of the microclimate.
It is not only about maintaining air purity, but also about maintaining the temperature regime. Microclimate indicators directly affect a person’s condition, body temperature, etc.

During the planning of microclimate indicators, the location of the medical institution, its number of storeys, as well as the types of patients that will be kept in the hospital, are taken into account.
For example, in operating rooms and postoperative, as well as postpartum wards, the optimal temperature is 21-24 degrees Celsius. And for rooms where any manipulations with newborns are performed, an indicator of 24 degrees is considered ideal.
Conclusions and useful video on the topic
In order to better understand the principle of the organization of ventilation, you can familiarize yourself with the tips that are given on the video:
Thus, ventilation in medical institutions must necessarily meet the standards and requirements that are imposed by the state.
These rules exist not only as bureaucratic difficulties designed to complicate the life of builders, but also as a guarantee of the life and health of all visitors and workers. Any deviation from these standards may entail a danger to the life and health of both doctors and patients.
If you have questions about the topic of the article or you can supplement the material with valuable information, please leave your comments in the block below.

 Arrangement of ventilation to the ceiling: types of ventilation systems and features of their arrangement
Arrangement of ventilation to the ceiling: types of ventilation systems and features of their arrangement  Cleanroom ventilation: design and installation rules for ventilation systems
Cleanroom ventilation: design and installation rules for ventilation systems  Ventilation of a room with gas-using equipment: design standards + arrangement rules
Ventilation of a room with gas-using equipment: design standards + arrangement rules  Forced ventilation in the cellar: rules and arrangements
Forced ventilation in the cellar: rules and arrangements  Natural ventilation in a private house: rules for arranging a gravitational air exchange system
Natural ventilation in a private house: rules for arranging a gravitational air exchange system  The rate of air exchange in the gym: the rules for arranging ventilation in the gym
The rate of air exchange in the gym: the rules for arranging ventilation in the gym  How much does it cost to connect gas to a private house: the price of organizing gas supply
How much does it cost to connect gas to a private house: the price of organizing gas supply  The best washing machines with dryer: model rating and customer tips
The best washing machines with dryer: model rating and customer tips  What is the color temperature of light and the nuances of choosing the temperature of the lamps to suit your needs
What is the color temperature of light and the nuances of choosing the temperature of the lamps to suit your needs  Replacement of a geyser in an apartment: replacement paperwork + basic norms and requirements
Replacement of a geyser in an apartment: replacement paperwork + basic norms and requirements